Part 1 of 2.
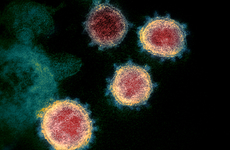
NEW YORK – As the SARS-CoV-2 virus ripped through the world like a wildfire in early 2020, the US was desperate for diagnostic tests to tame what would become the most devastating global health crisis in a century.
No one could predict what path the crisis would take, but producing homegrown, locally manufactured tests that could be used in diverse settings was the ultimate goal. Against that backdrop, the US National Institutes of Health rose to the moment. With $1.5 billion from the federal government, the institutes created a novel funding mechanism — the Rapid Acceleration of Diagnostics initiative, or RADx, comprising four subprograms with an overarching intention of developing, scaling, and implementing a diversity of diagnostic tests for COVID-19.
Two-and-a-half years later, RADx continues to help its portfolio of primarily assay developers and device makers achieve the milestones it created. Most recently, the program announced a round of solicitations that will most likely be its last, as there are no proposals to extend RADx's funding in the future.
But since the first round of RADx grants were awarded in July 2020, what has been achieved with all that funding? Did the program accelerate US diagnostic development, increase the diversity of available testing, onshore test manufacturing, save lives, or hasten the exit from a long and terrifying public health crisis? Were $1.5 billion in public funds invested wisely, and did the investments yield a strong return?
The answers may depend on how success is defined and the time frame allotted for achieving end goals, all the while accounting for flexibility in the face of evolving and novel circumstances.
The overall RADx investment portfolio clearly increased test availability in the US, primarily through scaling up lab-based services and rapid antigen testing. Specifically, RADx boasts it directly supported the cumulative production of 5 billion COVID-19 tests. Its support of more than 100 companies and academic labs led to 46 US Food and Drug Administration Emergency Use Authorizations of COVID-19 tests, including one for the first over-the-counter (OTC) diagnostic test for the disease.
And, although few of the novel devices that RADx supported have seen large volumes in sales, most are now at a stage of development where they could be adapted for other diseases and scaled up quickly, if and when the next global pandemic comes along.
Along with the success stories, there are tales of some firms that stumbled: In spite of the RADx support, some never received EUAs for their COVID-19 tests. And the experiences of a handful of companies — such as Ellume, Talis Biomedical, and Tangen Biosciences — may cast doubts on the wisdom of those particular investments.
Bruce Tromberg, director of the National Institute of Biomedical Imaging and Bioengineering (NIBIB), was given the responsibility of running the RADx program. He and other RADx representatives insist that the program will continue to try to make all the unique technologies it supported successful in the future.
An initial $500 million chunk of the RADx budget was earmarked for NIBIB, in part, to support a subprogram called RADx-Tech to spur development of at-home, point-of-care, and lab-based testing. The effort would also draw extensively on NIBIB's dozen or so years of experience coordinating the Point of Care Technology Research Network, or POCTRN.
Now, NIBIB is partnering with other NIH institutes to apply the overall RADx approach to other healthcare issues, supported by the institutes' own core budgets.
In a recent interview Tromberg said that although he is admittedly biased, the RADx portfolio, on balance, has been a success.
"It increased the testing capacity for the country, changed the conversation to over-the-counter tests … and helped people understand how to use them," he said.
In addition, "We built a lot of the pathways and structures that are instrumental in the overall national testing response and, I think, will be foundational for the future," Tromberg said.
Paradigm shifts
Besides the lofty goal of rapidly ramping up available testing and spurring new diagnostics approaches, RADx sought from the outset to be a different model of support.
Ultimately, the RADx program precipitated shifts in the way NIH and the FDA interact, as well as the pace and cadence of funding goals and milestones. It also changed the frequency and intensity of the interaction between funder and award recipients and the long-term expectations for investments.
Steve Schachter, a professor of neurology at Harvard University associated with POCTRN and the Consortia for Improving Medicine with Innovation and Technology (CIMIT), oversaw the rollout of RADx.
Overall, the program was "not at all typical for NIH," he said in an interview, both in the goals it set as well as the processes it used. Schachter coordinated a team of hundreds of experts — almost exclusively virtually — and was charged with setting a cultural tone and getting products to the market within a year.
"This program was so new, there were so many elements that we had to build before we needed them; it was like trying to build a plane as you're flying it," he said. Yet, the team was committed to the idea that everyone could work in complementary ways, drawing on their experience, judgment, and collegiality.
Compared to typical US federal funding for diagnostics development, RADx was faster, riskier, and more expensive. This entrepreneurial spirit was balanced by intensive mentoring, milestone-based fund dispersal, and de-risking strategies that included helping to secure end markets for fund recipients.
"Manufacturers won't make things unless they have confidence that there is a market," Tromberg said, so RADx worked hand in hand with the Administration for Strategic Preparedness and Response (ASPR), the US Department of Health and Human Services' Biomedical Advanced Research and Development Authority (BARDA) program, and the US Department of Defense (DoD) to secure test orders. RADx also helped with supply chain troubles, he said, including by invoking the Defense Production Act.
One of the more novel RADx processes included an innovation funnel that encouraged applicants to easily convey ideas and go through an intensive initial screening. Tromberg referred to this as "a foundational piece" of the RADx approach, involving a process reminiscent of the television show "Shark Tank." The final assessment, he said, was "a deep dive of hundreds of person-hours, with teams providing support" to dig into aspects such as the applicant's technology and commercialization strategies.
As the support teams gave responses to each company, a tight feedback loop was established, where developers and RADx could work to optimize the products, Tromberg explained. According to Schachter, this feedback included meetings every week, sometimes more frequently during certain crucial times.
Another novel aspect was the RADx Test Verification Core. Meant to "test the tests," the TVC included prominent academic researchers from many disciplines who executed a breathtaking amount of coordination and test evaluation. The TVC group has described its efforts as "a model for progress and change" and recently published its methods to confirm the accuracy of antigen tests in the context of evolving viral variants.
A major end goal in the commercialization process for many of the products that RADx supported was to obtain EUA from the FDA. The program provided developers intensive guidance in the EUA process and coordinated with the FDA to help establish the metrics by which tests should be evaluated.
For example, RADx developed a clinical studies core cited at the University of Massachusetts that Tromberg said was "absolutely critical" in helping to understand the use of serial testing paradigms for at-home rapid antigen testing, which ultimately became the FDA's standard for screening tests in May 2021.
RADx also collaborated with the US Centers for Disease Control and Prevention to launch a program called Say Yes! Covid Test in March 2021 aimed at assessing the utility of home testing and helped enable the FDA to prioritize submission of OTC home tests via its Independent Test Assessment Program, or ITAP, which launched in October 2021.
The paradigm shift in the at-home diagnostics landscape has been particularly seismic. The RADx team had a deeply held conviction that at-home testing would be needed for COVID-19, but as of April 2020, only one company had ever obtained US regulatory authorization for a home-use infectious disease test.
Indeed, as recently as 2019, at-home, OTC diagnostic testing for infectious diseases was even considered a bit scandalous in the eyes of some laboratorians, and developers faced commercialization challenges. Although there were theoretical health benefits to not having sick people traveling about seeking care — and groups like POCTRN had been pushing at this frontier for more than a decade — proving that an average citizen could successfully perform a diagnostic test and interpret the results remained a seemingly insurmountable hurdle.
Now, untold millions of COVID-19 rapid antigen assays have been run in US households. Tests that used to require personal protective equipment and at least some minimal healthcare training are run on coffee tables and kitchen counters. Parents hurriedly swab and test small children before school in the morning, and one recent study even demonstrated that children as young as 4 years old can adequately swab their own noses.
Tromberg credits the RADx team with helping to guide the US at each stage in this diagnostics paradigm shift — from having limited testing, to only lab tests, to growing point-of-care test availability, and, finally, to large-scale use of home testing.
And, RADx has now helped scale point-of-care and at-home test manufacturing capacity to more than 500 million tests per month, with cumulatively about 6 billion tests manufactured to date including 2 billion enabled through the ITAP program. Tromberg said this massive volume of testing was able to make a significant contribution to US public health.
All these efforts ultimately gave the White House the confidence to announce the free distribution of 1 billion at-home tests last year and early this year.
"That is all built around our programs and activities," Tromberg said.
Risky business
RADx also employed other novel strategic approaches, many of which carried significantly more risk than typical funding mechanisms.
The RADx team hypothesized early on that the timeline between a beta product and large-scale manufacturing could be compressed from years to months by carrying out the stages of diagnostics commercialization in parallel. This might look like validating a test as the device design was still being finalized, for example, or building out an automated assembly line while clinical trials were still ongoing.
This strategy increased risk, since it could lead to increased costs if, say, a device required a redesign after the manufacturing was already planned out.
There was also a risk that the end markets for the tests — hospitals, clinics, and the American public — might not be interested in some of the devices that RADx was funding, such as at-home rapid antigen tests.
Todd Merchak, co-program lead for RADx-Tech, said in a recent interview that the team was well aware it was taking more risks than usual. And so, "we set up a process that would help us reduce risk in the face of needing to move extremely quickly," he said.
Unlike typical Small Business Innovation Research support or venture capital, the RADx process included the intensive collaboration between developers and the RADx team, as well as in-kind support — everything from mentoring with expert consultants knowledgeable about device design, clinical trials, regulatory submissions, and manufacturing to supply chain negotiation and guidance with quality control.
The RADx funding was also dependent on achieving milestones, which Merchak and Tromberg both noted helped take some of the risk out of the investment.
In a typical SBIR — a program which actually almost missed reauthorization this year after its return on investment was scrutinized — funding is provided upfront with no milestones and no mentoring or other in-kind support. A venture portfolio, on the other hand, aims to winnow a portfolio down to the most successful investments and cut ties with ones that struggle, Tromberg said.
Merchak noted that SBIR success is usually measured by regulatory clearance and commercialization, with a success rate of 20 to 30 percent considered "pretty darn good." That was roughly the expectation for the RADx portfolio at the outset, he said, but by his estimation, the success of the RADx portfolio is well above 50 percent.
This is because "we set up the process to do a lot more diligence than would normally be done to understand all the risks across all the verticals — from business, to technology, to clinical, to market — to really understand whether or not this was a wise investment," Merchak said.
That process worked, he said, with the one caveat being that the biggest risk turned out to be FDA regulatory requirements. On the other hand, Emergency Use Authorization lowered the bar compared to 510(k), making clinical trials a little less burdensome, he said.
Tromberg also noted that the risk was high for developers, as well. "Everyone in industry has to think of a recurring revenue stream for their tests," but, he said, a niche test may make sense on the bottom line if the cost to get to a commercial stage is lowered by federal investment.
A bird's-eye view
RADx launched in April 2020, five days after its budget of $1.5 billion was authorized by Congress. At that point, the US was performing fewer than 1 million tests per month, Tromberg said.
All told, the program received more than 3,000 inquiries, received 824 complete submissions, and evaluated 179 in its "Shark Tank" process. Approximately 47 projects received Phase I funding for validation work, while 50 were awarded Phase II funding to support trials and regulatory submission and commercial scale-up. The awardee lists for the phases did not totally overlap, although some Phase I awardees did advance to Phase II.
The RADx program was divided into four units. RADx Advanced Technology Platforms, or RADx-ATP, had a budget of $230 million to scale up technologies that were already in use. The RADx Underserved Populations, or RADx-UP, program used $500 million to enhance testing in vulnerable communities, while the RADx Radical, or RADx-Rad, program used $200 million to support non-traditional testing methods and approaches.
The RADx-Tech set out to invest $500 million in rapid home and point-of-care testing via a competitive three-phase challenge.
This meant supporting different types of testing technologies, including PCR, isothermal nucleic acid amplification, sequencing, and antigen tests, as well as emerging technologies like CRISPR and biosensors. It also meant supporting different use cases from high-throughput tests run in large labs down to single-use, disposable home tests.
For example, in its Phase II awards RADx-Tech and RADx-ATP together supported five OTC tests, 26 point-of-care tests, and 16 lab-based tests, allocating approximately $262 million for 18 rapid antigen testing technologies and $417 million to support 28 different molecular diagnostic technologies.
September 2020 was the first hard deadline for the program to enable a safer back-to-school and back-to-work transition and head off the possibility of co-occurring flu and COVID surges.
"We had to make an impact in five months," Tromberg said. And so, at the beginning, "we tried to put investment into [products] that could go the fastest and be the most impactful and fill a space that was not being filled."
Schachter said that with all of the use cases that the program envisioned — from a lab, to a hospital, to the home, to "a remote fishing village in Alaska" — there was no one set of specifications for a COVID-19 assay that would make it ideal in every setting.
"There wasn't going to be a single, one-size-fits-all, diagnostic test," he said. In addition, there was no way to know which of the technologies would prove to be accurate and commercializable.
And so, RADx took the approach of funding multiple projects in parallel, "so there would be a diversity, and likely be at least one product that was appropriate for every use case," Schachter said.
The end goals the program set for itself also shifted along the way as the pandemic evolved, he said.
Initially, the intent was to support companies and academic groups in developing commercializable diagnostics for COVID-19. But, Schachter said, it became apparent over time that "to do a complete job we needed to take these products all the way through manufacturing, FDA EUA, and even delivery to the end user."
Tromberg said the RADx team also helped introduce innovation in the regulatory process itself, "so that when the final module that the FDA needed to see came in, they could make a decision on the EUA the next day."
And, to support home-use tests in particular, the RADx team determined that it needed to coordinate with the FDA and provide education in the form of public-facing websites.
According to Merchak, the initial goal of RADx was to increase the available lab testing capacity in the US, followed by getting point-of-care OTC tests to the market. The RADx team also had to stay nimble because "we couldn't totally model human behavior," and it was not clear what the public would be willing to do, he said.
"People took to the home testing pretty quickly, and that overtook other forms of testing," he said. The Delta surge around the middle of 2021 and Omicron surge at the end of 2021 accelerated the need for home tests, and the Biden administration rolled out the procurement initiatives that provided a billion free tests to the public.
"This was changing from month to month, as we were understanding variant dynamics and the numbers of cases," Merchak said, and these ebbs and flows also made manufacturing the right number of tests to meet demand quite tricky.
Clear wins
By July 2021, the US had scaled up capacity to perform nearly 5 million COVID tests per day. And, including home testing, there were 1 billion COVID-19 tests performed in February 2022, Tromberg said, a significant increase from the fewer than 1 million COVID tests performed in April 2020.
Considering the high-level economic benefits of RADx, Schachter said it might be useful to think of the impact the program had in allowing people to work, knowing they were healthy, or conversely making sure they didn't go to work because they knew they had COVID-19. The program also created new jobs and led to follow-on investment in the companies that RADx supported.
Indeed, companies that participated in the RADx program often benefited in ways beyond the immediate funding they received. For example, RADx awarded San Francisco-based Helix $33.4 million for amplicon sequencing-based high-throughput testing. The firm obtained EUA in August 2020, and it subsequently raised $50 million in Series C financing. More recently it was awarded approximately $900,000 from the Rockefeller Foundation's Pandemic Prevention Institute for viral surveillance.
RADx also awarded Ginkgo Bioworks $40.5 million for a high-throughput next-generation sequencing test. A spokesperson said the Boston-based company found that RADx aligned well with its Concentric biosecurity and public health arm it had established in 2020 and noted that its rapid scale-up was supported through the RADx-ATP program.
The support Ginkgo received from program managers and subject matter expert mentors was "tremendous," according to the spokesperson. Along with partner labs, Ginkgo claims to have tested more than 10 million samples for SARS-CoV-2, particularly for K-12 schools. The support also had the added benefit of helping Ginkgo advance its automated cell programming platform, and it is now building a global biosecurity infrastructure with expanded pathogen detection and analytics capabilities and new modalities like air and wastewater sampling.
For rapid antigen testing, RADx awarded Becton Dickinson $457,000 to scale its Veritor immunoassay system and help perform post-market studies for COVID-19 diagnostic tests, according to a spokesperson. The BD Veritor test received EUA in July 2020, followed by over-the-counter authorization for serial testing. HHS quickly purchased 2,000 Veritor systems and 750,000 COVID assays. And, along with the DoD, HHS has supported further manufacturing scale-up with a $24 million award. By early 2021, BD had tripled the installed base of Veritors to 70,000 instruments, got EUA for an at-home test, and was awarded additional funding from BARDA for a combination COVID/flu test on Veritor.
Similarly, RADx awarded QuidelOrtho $70.5 million to scale up manufacturing of its Sofia immunoassays. It received the first EUA for a COVID-19 rapid antigen test in May 2020, followed by an EUA for at-home testing in March 2021. In the interim — and perhaps emblematic of the trouble much of the industry faced — QuidelOrtho had to delay EUA submission for the OTC test because COVID-19 cases were in an ebb phase. QuidelOrtho did not respond to requests for comment, but Tromberg said RADx funding enabled the firm to quickly scale Sofia manufacturing to 20,000 tests per day.
QuidelOrtho also received $717,800 from RADx to develop an over-the-counter flu and COVID combination test, and a respiratory viral panel on the Savanna molecular diagnostics system. For the first quarter of 2022, the San Diego-based firm reported its rapid immunoassay product revenues increased by $655.1 million year over year, mostly due to OTC test sales during the Omicron wave. Some of these successes likely also supported Quidel's acquisition of Ortho Clinical Diagnostics for $6 billion in December 2021, creating the merged QuidelOrtho firm.
Much of the portfolio supported by RADx was able to reach the EUA milestone. According to RADx's count, 39 technologies it supported obtained EUA, along with an additional six technologies whose regulatory authorizations were enabled by ITAP assessment. Six firms supported by RADx were allowed to perform testing under umbrella authorizations or lab-developed test emergency authorizations, for example, by using Thermo Fisher Scientifics' TaqPath test or the Yale SalivaDirect protocol.
Nashville, Tennessee-based clinical lab Aegis Sciences, for example, used the Thermo Fisher TaqPath COVID-19 Combo Kit in accordance with the manufacturer's EUA authorization, according to its website. RADx awarded Aegis $6.6 million for diagnostic testing, and it scaled its RT-qPCR service from 3,500 tests per day in April 2020 to 60,000 per day by the end of September, according to Aegis. The company also formed a partnership with Walgreens pharmacy and said it has performed 14 million tests to date.
Brooklyn-based Mirimus was a designated lab under the Yale SalivaDirect protocol and performed testing for public schools in New Jersey and Westchester County in New York. RADx awarded Mirimus $1 million for high-throughput pooled saliva testing, and Mirimus subsequently was one of six winners of the XPrize competition for innovative technologies.
For RADx's Schachter, a high point of all these successes was that they proved the RADx process worked.
"It showed you could combine the best of academic and the best of business practices in finding funding and facilitating medical technology projects, in a way that might be more productive than an SBIR program," he said. This was directly related to the fact that RADx "required such intense and close mentoring," but also set high bars in terms of speed to market.
While he remains impressed so many of the companies RADx supported were successful, nevertheless, "the nature of technology development is that not everything makes it to the goal line," he said.
RADx funded all the companies and academic labs in its portfolio because after extensive due diligence, it had a strong belief that the technologies were novel and could address unmet needs.
But, "there are many reasons why those plans might not come to fruition," Schachter said.
Part 2 of this story will look at some of the less successful RADx investments, the program's support of novel device makers, and its future directions.
